Understanding Asperger’s Syndrome: Insights into a Unique Neurodevelopmental Condition
Asperger’s Syndrome is a developmental disorder characterized by challenges in social interaction and rigid, repetitive behavior and thinking patterns.
Children and adolescents with Asperger’s Syndrome generally have the ability to communicate verbally and perform reasonably well academically. However, they struggle with comprehending social situations and subtle forms of communication such as body language, humor, and sarcasm. They may exhibit a tendency to focus excessively on one particular topic or interest and prefer a limited range of activities. These intense interests can become all-consuming and disrupt daily life.
Symptoms
The symptoms of Asperger’s Syndrome include difficulties in social interactions, obsessions, unusual speech patterns, limited facial expressions, and other distinctive mannerisms. Children with Asperger’s Syndrome may engage in repetitive routines and display heightened sensitivity to sensory stimuli.
While every child with Asperger’s Syndrome is unique, their notable traits lie in their atypical social skills and fixated interests. When observing a child with Asperger’s Syndrome, one may notice one or more of the following symptoms:
- Inappropriate or minimal social interactions
- Conversations that almost always revolve around themselves or a certain topic, rather than others
- Not understanding emotions well or having less facial expression than others
- Speech that sounds unusual, such as flat, high-pitched, quiet, loud, or robotic
- Not using or understanding nonverbal communication, such as gestures, body language and facial expression
- An intense obsession with one or two specific, narrow subjects
- Becoming upset at any small changes in routines
- Memorizing preferred information and facts easily
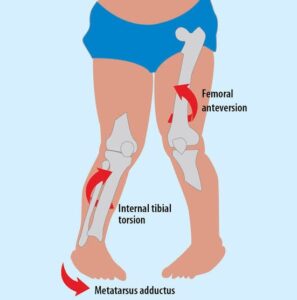
- Clumsy, uncoordinated movements, including difficulty with handwriting
- Difficulty managing emotions, sometimes leading to verbal or behavioral outbursts, self-injurious behaviors or tantrums
- Not understanding other peoples’ feelings or perspectives
- Hypersensitivity to lights, sounds and textures
Children with Asperger’s Syndrome typically demonstrate normal language development without significant delays. They often exhibit strong grammar skills and possess an extensive vocabulary. However, their use of language may be characterized by a literal interpretation of meaning, making it challenging for them to navigate social contexts effectively.
Regarding cognitive development, there is typically no noticeable delay in children with Asperger’s Syndrome. While they may struggle with attention span and organization, their intelligence quotient (IQ) tends to fall within the average range.
Causes
- The causes of Asperger’s Syndrome are unknown.
- Genetics and brain abnormalities may be involved.
- We do know that Asperger’s Syndrome is NOT the result of a child’s upbringing or poor parenting.
- It is a neurobiological disorder, meaning it is just a part of the child’s brain development, whose causes are not fully understood.
Treatment
Treatment usually includes:
- Social skills training
- Behavior supports
- Cognitive behavioral therapy
- Parent education and training
- Speech-language therapy
- Occupational therapy
Physiotherapy Treatment

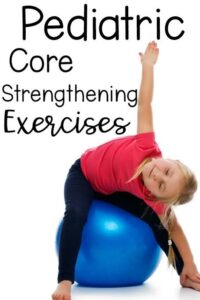
- Physical therapy for individuals with Asperger’s Syndrome primarily focuses on improving gross motor skills such as crawling, sitting, rolling, walking, and running.
- As children with Asperger’s Syndrome grow older, physical therapy may involve more advanced tasks like jumping, stair climbing, throwing, and catching.
- These motor skills are crucial for both physical development and active participation in play and sports.
- During physiotherapy sessions, the individual’s physical abilities will be assessed and evaluated to determine the nature and extent of any challenges, leading to the formulation of an appropriate treatment plan.
- The physiotherapist will develop a personalized treatment plan based on the individual’s specific needs and abilities.
- Physiotherapy will encompass a range of exercises and therapeutic programs aimed at improving physical abilities, coordination, and balance.
- Collaboration between physiotherapists and educational professionals is vital to ensure awareness of any gross motor skill challenges and to provide effective strategies and interventions for managing these difficulties.