Empowering Women Through Pelvic Floor Physiotherapy: Navigating Menopause With Confidence
Title: “Navigating Menopause with Pelvic Floor Physiotherapy: Prioritizing Women’s Wellness”
Introduction:
Menopause is a significant natural phase in a woman’s life, signifying the end of her reproductive years. While it is a momentous transition, it is accompanied by various physical and hormonal changes, some of which can impact a woman’s pelvic health. Pelvic floor physiotherapy has emerged as a vital component in addressing the challenges that menopause may bring.
Understanding Menopause and Its Implications:
Menopause typically occurs between the ages of 45 and 55 when a woman’s ovaries cease to produce eggs, leading to a decline in estrogen and progesterone hormones. This hormonal shift can result in a range of symptoms, including hot flashes, mood swings, and alterations in vaginal health.
Effects on Pelvic Health:
Menopause can influence pelvic health in multiple ways:
- Vaginal Dryness and Atrophy: Diminished estrogen levels can lead to vaginal dryness, thinning of vaginal walls, and reduced elasticity, causing discomfort, pain, and an increased susceptibility to vaginal infections.
- Urinary Incontinence: Changes in pelvic muscles and tissues can contribute to urinary incontinence, ranging from mild leakage to more severe issues.
- Pelvic Organ Prolapse: Weakened pelvic floor muscles may lead to the displacement of pelvic organs, such as the bladder, uterus, or rectum, resulting in discomfort or pain.
The Role of Pelvic Floor Physiotherapy:
Pelvic floor physiotherapy stands as a non-invasive and highly effective treatment option for addressing pelvic health challenges during menopause. Here’s how it can offer assistance:
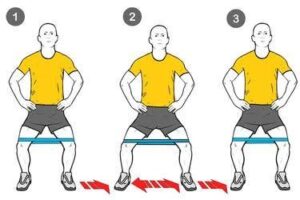
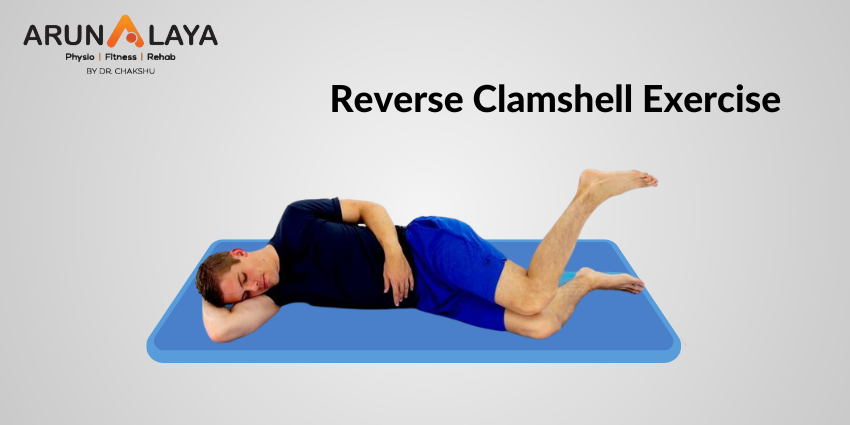
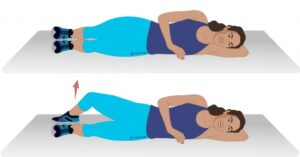
- Strengthening Pelvic Floor Muscles: A skilled pelvic floor physiotherapist can devise a personalized exercise regimen to fortify weakened pelvic floor muscles. These exercises can alleviate incontinence and enhance pelvic support.
- Education and Lifestyle Guidance: Women undergoing menopause can greatly benefit from expert counsel on managing their pelvic health through lifestyle adjustments, encompassing diet, hydration, and exercise.
- Techniques for Vaginal Health: Pelvic floor physiotherapists can educate women on techniques for maintaining vaginal health, including the utilization of vaginal moisturizers and dilators.
- Pain Management: For women enduring pelvic discomfort or pain, physiotherapy can offer relief through manual techniques and tailored exercises.
Conclusion:
Menopause represents a transformative stage in a woman’s life, and it need not be synonymous with discomfort or pain. Pelvic floor physiotherapy embraces a holistic approach to managing pelvic health concerns associated with menopause, allowing women to regain control and live their lives comfortably and confidently. Seeking the guidance of a qualified pelvic floor physiotherapist empowers women to gracefully navigate this phase with vitality and well-being.