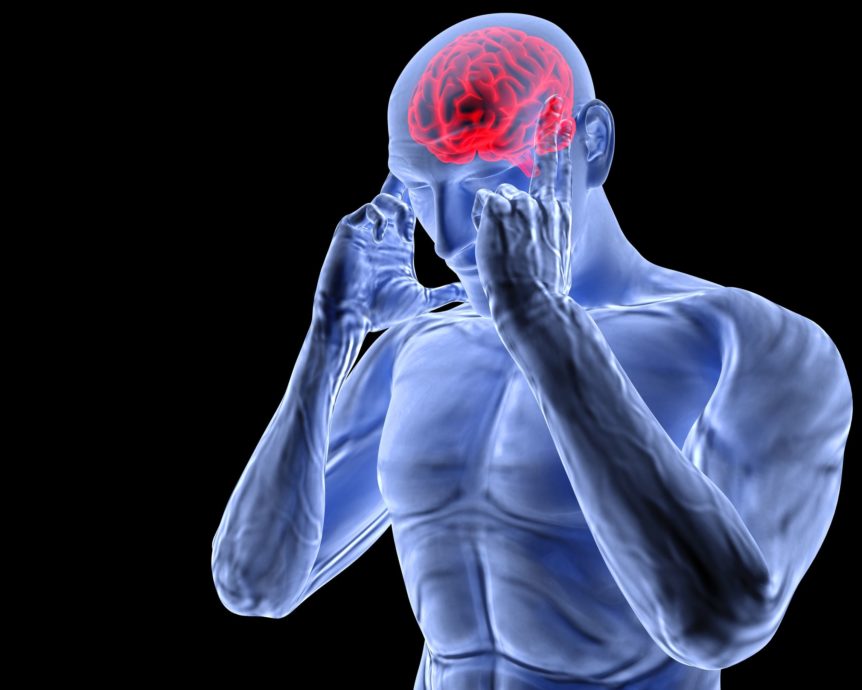
Headache
Table Of Contents
- Introduction
- Exploring the Complexity of Headaches
- Identifying the Signs and Symptoms
- Effective Relief Strategies for Headaches
- Preventing Headaches
- Conclusion
Introduction
Headaches are a common and often disruptive condition that can occur for a variety of reasons, ranging from tension and stress to underlying medical conditions. Whether it’s a dull ache or a throbbing pain, headaches can significantly impact daily activities and quality of life. In this blog post, we’ll delve into the causes, symptoms, and effective relief strategies for headaches, offering insights into how you can find relief and regain control of your head health.
Exploring the Complexity of Headaches
Headaches can arise from various factors, including:
- Tension headaches: Often caused by muscle tension in the head, neck, and shoulders, tension headaches can result from stress, poor posture, or anxiety.
- Migraines: Migraine headaches are characterized by intense throbbing or pulsating pain, often accompanied by other symptoms such as nausea, sensitivity to light and sound, and visual disturbances.
- Cluster headaches: Cluster headaches are a rare but severe form of headache that occur in cyclical patterns, often lasting between 15 minutes to 3 hours and occurring multiple times a day.
- Sinus headaches: Sinus headaches result from inflammation or congestion in the sinuses, often due to allergies, infections, or environmental triggers.
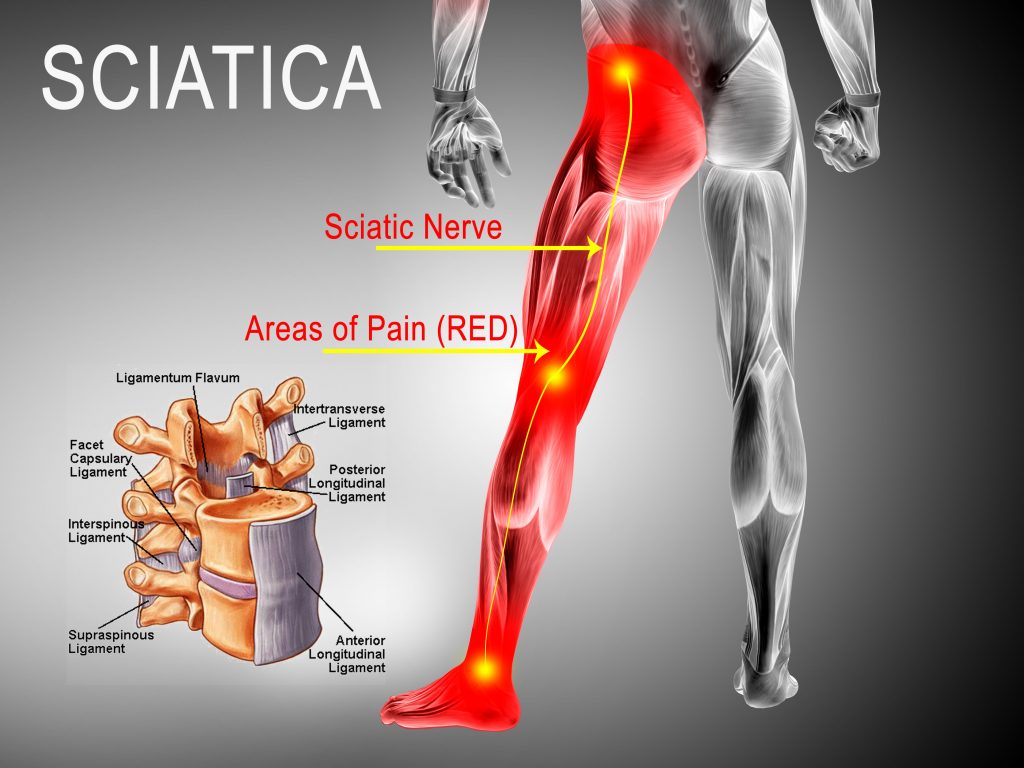
- Cervicogenic headaches: Cervicogenic headaches originate from issues in the cervical spine or neck, such as muscle tension, cervical disc herniation, or arthritis.
Identifying the Signs and Symptoms
The symptoms of headaches can vary depending on the type and underlying cause, but may include:
- Dull, aching pain or pressure in the head or temples
- Throbbing or pulsating pain on one or both sides of the head
- Sensitivity to light, sound, or odors
- Nausea or vomiting
- Visual disturbances, such as aura or flashing lights
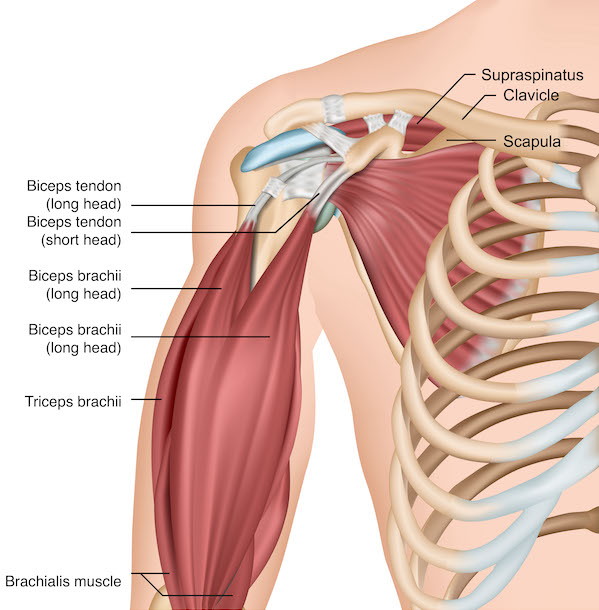
- Tenderness or stiffness in the neck and shoulders
- Difficulty concentrating or focusing
- Changes in mood or irritability
Effective Relief Strategies for Headaches
Treating headaches often involves a combination of lifestyle modifications, self-care techniques, and medical interventions, including:
- Managing stress: Practicing relaxation techniques, such as deep breathing, meditation, or yoga, can help reduce muscle tension and alleviate headache symptoms.
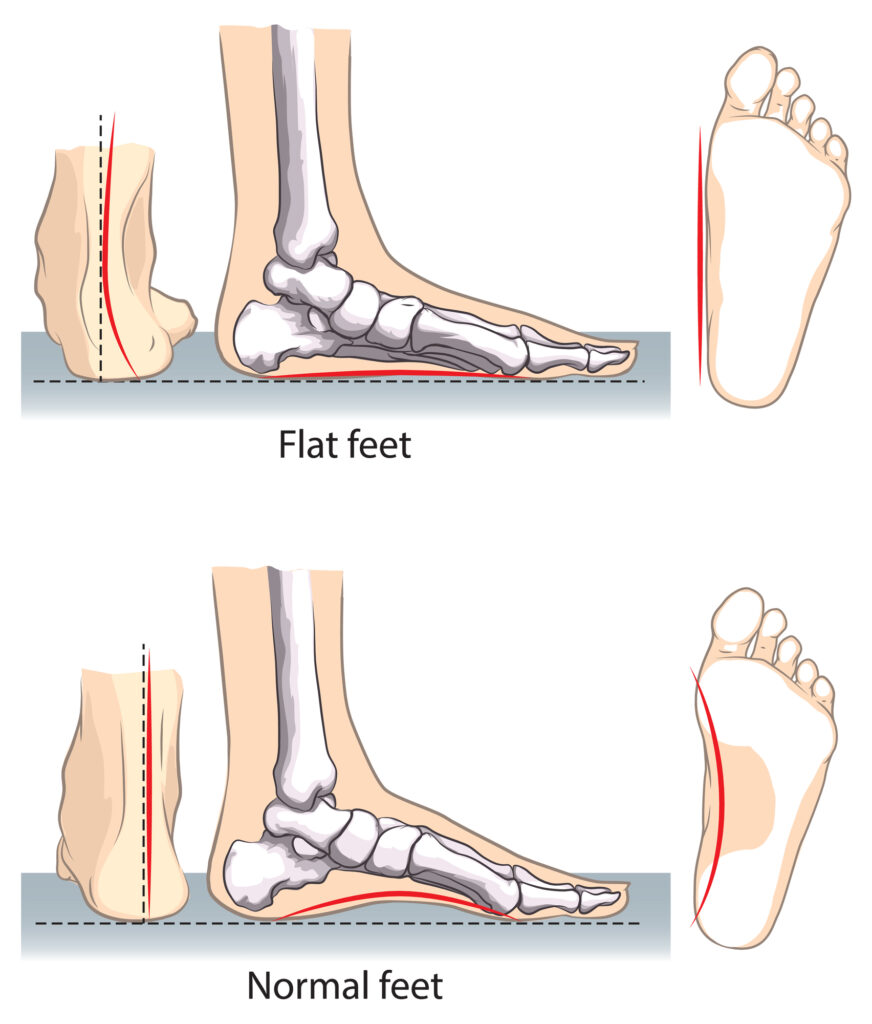
- Improving posture: Maintaining proper posture when sitting, standing, or working can reduce strain on the muscles and joints of the head and neck.
- Getting adequate sleep: Establishing a regular sleep schedule and ensuring sufficient rest can help prevent headaches triggered by sleep disturbances or fatigue.
- Hydrating properly: Drinking plenty of water throughout the day can help prevent dehydration, a common trigger for headaches.
- Avoiding triggers: Identifying and avoiding potential headache triggers, such as certain foods, environmental factors, or hormonal changes, can help prevent headaches from occurring.
- Using over-the-counter pain relievers: Nonprescription medications, such as acetaminophen, ibuprofen, or aspirin, can help alleviate mild to moderate headache pain.
- Applying heat or cold therapy: Applying heat packs or cold compresses to the head or neck can help reduce muscle tension and alleviate headache symptoms.
- Seeking medical treatment: If headaches persist or worsen despite self-care measures, it’s important to seek evaluation and treatment from a healthcare professional, who can provide personalized recommendations and interventions.
Preventing Headaches
While it may not always be possible to prevent headaches entirely, there are steps you can take to reduce their frequency and severity, including:
- Practicing good ergonomics and posture
- Managing stress through relaxation techniques and stress-reducing activities
- Maintaining a healthy lifestyle with regular exercise, balanced nutrition, and adequate hydration
- Avoiding known headache triggers, such as certain foods, beverages, or environmental factors
- Establishing a consistent sleep schedule and prioritizing sufficient rest
Conclusion
Headaches can be a challenging and disruptive condition, but with the right approach, they are often manageable. By understanding the causes, symptoms, and effective relief strategies for headaches, you can take proactive steps to address your symptoms and improve your head health. If you’re experiencing persistent or severe headaches, don’t hesitate to seek evaluation and treatment from a qualified healthcare professional. With proper care and management, you can find relief from headaches and regain control of your life.
“At Arunalaya Healthcare, we pride ourselves on being the best physiotherapy center in Delhi. Our dedicated team of experts offers top-notch physiotherapy treatment tailored to your needs. Experience the difference with the leading physiotherapy clinic in Delhi area. Our commitment to excellence ensures that you receive the best physiotherapy care possible. Trust Arunalaya Healthcare for the best physiotherapy treatment in Delhi. Our advanced physiotherapy solutions set us apart as the premier choice for your rehabilitation needs. When it comes to physiotherapy, our center stands out as the best in Delhi. Choose Arunalaya Healthcare for comprehensive physiotherapy solutions that deliver results. Visit Arunalaya Healthcare today and discover why we are the best physiotherapy center in Delhi.”
Headache relief tips | Causes of migraines and tension headaches | Symptoms of cluster headaches | How to treat sinus headaches | Cervicogenic headache management | Natural remedies for headache relief | Hydration tips for headache prevention | Headache triggers and how to avoid them | Posture improvement for headache reduction