
A Brief About Jersey finger
Jersey finger, a challenging injury common in athletes, especially in sports like American football and rugby, can be debilitating. This injury occurs when the flexor tendon, often affecting the ring finger, is forcibly extended, causing pain and limited function. Physiotherapists play a vital role in the rehabilitation journey post-jersey finger repair surgery. In this article, we present a detailed guide to the rehabilitation protocol, including exercises and advanced techniques, to assist physiotherapists in effectively managing this complex injury.

Rehabilitation Phases
Rehabilitating jersey fingers involves three critical phases: early, intermediate, and advanced, each tailored to specific goals and exercises to ensure a successful recovery.
Phase I:
Early Rehabilitation (0-4 Weeks Post-Surgery) In the initial phase, the focus is on pain management, wound healing, and safeguarding the repaired tendon.
- Edema Control: Managing post-operative swelling through cryotherapy and elevation, supplemented by gentle manual lymphatic drainage techniques.
- Passive Range of Motion (ROM): Gentle passive finger flexion and extension to maintain joint mobility while protecting the repair site.
- Tendon Gliding Exercises: Encouraging tendon gliding exercises multiple times a day to prevent adhesions, including active and passive flexion and extension.
- Scar Management: Teaching scar massage techniques and recommending silicone gel sheets to promote healing and prevent adhesions.
- Strengthening: Initiating isometric strengthening of the wrist and forearm to maintain muscle tone without overloading the repaired tendon.
Phase II:
Intermediate Rehabilitation (4-8 Weeks Post-Surgery) This phase shifts the focus towards improving finger strength, flexibility, and functional abilities.
- Active Range of Motion: Encouraging active finger flexion and extension, gradually increasing the range.
- Strengthening: Incorporating resistance exercises using putty, handgrip devices, and resistance bands to enhance finger flexor and extensor strength, emphasizing eccentric strengthening.
- Functional Activities: Introducing activities like gripping objects, opening and closing doors, and typing to simulate real-world demands.
- Proprioception and Sensory Awareness: Employing proprioceptive exercises, such as tactile recognition of various textures or objects blindfolded, to improve sensory feedback.
Phase III:
Advanced Rehabilitation (8+ Weeks Post-Surgery) In the final phase, the focus is on returning the patient to their pre-injury level of function, emphasizing sports-specific movements.
- Sports-Specific Drills: Tailoring exercises to the demands of the patient’s sport, involving activities like gripping sports equipment or tackling dummies.
- Plyometric and Isokinetic Training: Introducing plyometric exercises and isokinetic strength testing to assess the repaired tendon’s functional capabilities.
- Stretching: Incorporating static stretching to enhance finger flexibility and reduce the risk of reinjury.
- Neuromuscular Control: Implementing activities that challenge neuromuscular control, such as balance exercises on unstable surfaces.
- Functional Testing: Utilizing standardized functional tests like the Hand Sports Activity Test (HSAT) to evaluate the patient’s readiness for return to play.
Importance and Repetitions
Each exercise and technique in the jersey finger rehabilitation protocol is crucial for a successful recovery, addressing pain management, preventing adhesions, restoring function, and preventing re-injury. Repetition and progression should align with the patient’s individual progress and goals, with regular reevaluation and communication between the physiotherapist and surgeon for a safe and successful rehabilitation journey.
Conclusion
Rehabilitating jersey fingers is a multifaceted process requiring careful planning and execution by physiotherapists. This comprehensive protocol, spanning early, intermediate, and advanced phases, aims to guide physiotherapists in effectively managing this challenging injury. Patient compliance, gradual progression, and communication with the surgical team are paramount. By following these guidelines, physiotherapists can empower patients to regain optimal hand function and return to their sports and activities with confidence.
Lateral Ligament Injuries of the Ankle
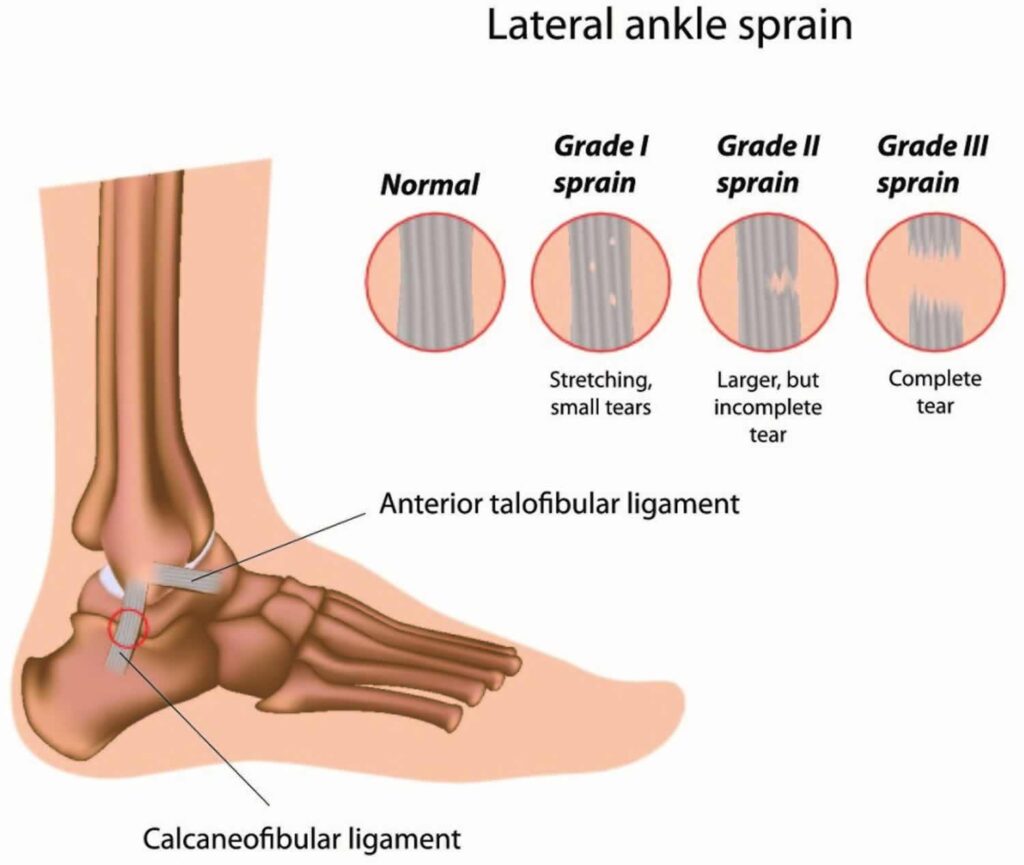
Lateral ligament injuries, often seen in athletes, are among the most prevalent sports-related injuries that physiotherapists encounter. These injuries, including lateral ankle sprains, affect both men and women at similar rates. A lateral ligament injury of the ankle arises when the ligaments on the outer side of the ankle endure damage. The primary ligaments involved are the anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), and posterior talofibular ligament (PTFL), which provide stability to the ankle joint.
Understanding Lateral Ankle Ligament Tears:
Lateral ligament injuries can be categorized into three types based on the ligaments affected and the severity of the tear:
- Anterior talofibular ligament (ATFL) injury: This is the most common type, often occurring in isolation. It involves stretching or tearing of the ATFL, which connects the talus bone to the fibula and is frequently associated with ankle inversion injuries.
- Calcaneofibular ligament (CFL) injury: Located slightly below the ATFL, the CFL connects the calcaneus (heel bone) to the fibula. CFL injuries often occur alongside ATFL injuries or in more severe sprains, sometimes resulting in higher-grade ligament tears.
- Posterior talofibular ligament (PTFL) injury: PTFL is the least frequently injured ligament in lateral ligament injuries. It connects the talus bone to the fibula at the back of the ankle and is usually damaged in severe ankle sprains or high-energy trauma.
Causes:
- Ankle sprain: The most common cause of a lateral ligament injury is an ankle sprain, typically resulting from the foot rolling inward, leading to stretching or tearing of the outer ankle ligaments.
- Sports injuries: Activities involving quick changes in direction, jumping, or running on uneven surfaces increase the risk of ankle sprains and ligament injuries.
- Trauma: Direct trauma or impact to the ankle joint, such as falls or collisions, can also cause damage to the lateral ligaments.
Clinical Features:
- Pain on the outer side of the ankle
- Swelling and bruising
- Difficulty walking or bearing weight on the affected foot
- Instability or a feeling of the ankle giving way
- Limited range of motion in the ankle joint
Assessment of Ankle Joint:
Assessing lateral ligament injuries involves evaluating the level of instability, loss of range of motion, muscle strength, and reduced proprioception. Observation of the foot and ankle for signs of injury, inflammation, or changes in the skin is crucial. Additionally, understanding the mechanism of injury and a patient’s injury history aids in diagnosis.
Grades of Lateral Ligament Tears: Lateral ligament injuries are categorized into three grades:
- Grade 1: Mild sprain with minimal stretching or tearing, causing slight swelling, tenderness, and minimal loss of function.
- Grade 2: Moderate sprain with partial tearing, leading to increased swelling, bruising, pain, and difficulty walking or bearing weight.
- Grade 3: Severe sprain with complete tearing or rupture, resulting in significant swelling, bruising, pain, and instability, making walking or weight-bearing extremely challenging.
Treatment:
The initial phase of treating a lateral ligament injury focuses on pain and swelling reduction through the RICE regimen (Rest, Ice, Compression, Elevation). Gentle soft tissue massage and pain-free stretching can aid in edema removal. Subsequent phases include range of motion, strengthening, proprioceptive, and balance exercises. Returning to functional activity requires achieving pain-free movement, normal strength, and proprioception. Athletes should consider wearing ankle support during sports for an additional six months after recovery.
Conclusion
Lateral ligament injuries of the ankle are common but manageable with proper care and rehabilitation. Understanding the severity of the injury and following a comprehensive rehabilitation plan under the guidance of a physiotherapist can empower individuals to regain optimal ankle function and confidently return to their regular activities.
Concussion Rehabilitation and Support

A concussion, a form of traumatic brain injury (TBI), occurs due to head trauma or sudden head movements, leading to the brain’s shaking within the skull. This can result in temporary brain cell dysfunction and manifest in various physical, cognitive, and emotional symptoms.
Understanding Concussion Symptoms: Concussion symptoms encompass a wide range of experiences and may include:
- Headache or head pressure
- Dizziness or balance issues
- Nausea or vomiting
- Blurred vision or light sensitivity
- Confusion or mental fogginess
- Memory problems or concentration difficulties
- Slurred speech or trouble speaking
- Fatigue or drowsiness
- Mood changes or personality shifts
- Sleep disturbances, either excessive sleepiness or difficulty sleeping
It’s important to note that not all concussions involve loss of consciousness. In fact, most do not.
Common Causes of Concussions:
- Sports Injuries: Contact sports like football, soccer, hockey, and more can lead to concussions due to player collisions or impacts with hard surfaces.
- Falls: Slip-and-fall accidents, particularly among the elderly and young children, are common causes of concussions.
- Vehicle Accidents: Car crashes, motorcycle, bicycle, or pedestrian accidents can result in head injuries and concussions.
- Assaults: Physical altercations and violent acts can lead to head trauma and concussions.
- Explosions or Blast Injuries: Military personnel and civilians exposed to explosions may suffer concussions, known as blast-related or mild traumatic brain injuries (mTBI).
- Home or Workplace Accidents: Any incident involving head impact, like falling objects or collisions with hard surfaces, can cause a concussion.
Grading Concussions: Concussions are graded based on severity:
- Grade 1: Mild concussion with transient confusion but no loss of consciousness. Symptoms typically resolve within 15 minutes.
- Grade 2: Moderate concussion with transient confusion and loss of consciousness lasting less than 5 minutes. Symptoms may persist for longer.
- Grade 3: Severe concussion with loss of consciousness for over 5 minutes and more pronounced and prolonged symptoms.
Prevention: Preventing concussions involves:
- Wearing appropriate protective gear in sports and high-risk activities.
- Adhering to safety guidelines and rules in sports and recreational pursuits.
- Maintaining safety standards and equipment in workplaces and construction sites.
- Incorporating safety features in vehicles to minimize head injuries during accidents.
Concussion Rehabilitation:
Concussion rehabilitation aims to aid individuals in recovering from concussions and effectively managing lingering symptoms. The primary objectives are to support the brain’s healing, restore function, and gradually reintegrate individuals into their pre-injury activities and lifestyles.
Key Components of Rehabilitation:
- Rest and Gradual Return to Activity: Initially, adequate rest is crucial to allow the brain to heal. Gradual reintegration of normal activities begins as symptoms improve, with close monitoring by healthcare professionals.
- Education and Counseling: Education about concussions and expected recovery, along with counseling to address emotional and psychological aspects, are vital components.
- Vestibular Rehabilitation: If the vestibular system (responsible for balance and spatial orientation) is affected, specialized therapy focuses on balance, coordination, and reducing dizziness.
- Vision Therapy: Vision disturbances post-concussion are addressed through exercises and treatments by optometrists or vision specialists.
- Cognitive Rehabilitation: Cognitive difficulties such as memory problems or attention issues are managed through exercises and strategies.
- Physical Therapy: Physical symptoms like headaches or muscular imbalances are relieved through manual therapy and exercises.
- Gradual Return to Play (For Athletes): Athletes follow a structured “Return to Play” protocol to ensure a safe return to sports.
- Academic Support: Students may receive academic accommodations to aid their recovery.
- Psychological Support: Counseling or psychotherapy may be recommended for emotional and psychological challenges.
- Vestibular Physiotherapy: Focuses on balance problems and dizziness resulting from vestibular system disruptions.
- Balance and Coordination Training: Exercises to improve proprioception and restore stability.
- Vision and Oculomotor Training: Addresses eye tracking and light sensitivity.
- Headache Management: Strategies for managing post-concussion headaches.
- Gaze Stabilization Exercises: Improve focus during head movement.
- Postural Control Training: Addresses postural stability and balance.
- Cardiovascular Conditioning: May be included to enhance overall endurance.
- Fatigue Management: Strategies for managing post-concussion fatigue.
Conclusion
Concussions require comprehensive care and rehabilitation to support individuals in their journey to recovery. Understanding the severity of the injury and following a tailored rehabilitation plan under the guidance of healthcare professionals empowers individuals to regain their optimal functioning and return to their regular lives with confidence.
