Lateral ligament injury is among the most prevalent types of sports injuries addressed by physiotherapists. Men and women are estimated to suffer from lateral ankle sprains at roughly the same rates.
A lateral ligament injury of the ankle is a common injury that occurs when the ligaments on the outer side of the ankle are damaged. The most frequently affected ligaments are the anterior talofibular ligament (ATFL), the calcaneofibular ligament (CFL), and the posterior talofibular ligament (PTFL). These ligaments are responsible for providing stability to the ankle joint.
Lateral ankle sprains are also known as inversion or supination ankle sprains. The complex of ligaments on the lateral side of the ankle is torn by varied degrees as a result of a forced plantarflexion/inversion movement.
Individuals who sustain multiple recurrent ankle sprains have been documented to have functional and mechanical instability, as well as an increased risk of re-injury. Small fractures surrounding the ankle and foot (e.g. Pott’s fracture) and straining or rupture of the muscles around the ankle (e.g. calf, peroneii, tibialis anterior) should also be avoided even if they are the less prevalent causes of ankle pain.
Lateral Ankle Ligament Tear Types:
Lateral ligament injuries of the ankle can be classified into three main types based on the ligaments involved and the severity of the tear:
Anterior talofibular ligament (ATFL) injury: This is the most common type of lateral ligament injury and often occurs in isolation. It involves the stretching or tearing of the ATFL, which connects the talus bone to the fibula. It is commonly associated with ankle inversion injuries.
Calcaneofibular ligament (CFL) injury: The CFL is located slightly below the ATFL and connects the calcaneus (heel bone) to the fibula. CFL injuries typically occur along with ATFL injuries or in more severe sprains. In some cases, the ATFL and CFL can be injured together, resulting in a higher-grade ligament tear.
Posterior talofibular ligament (PTFL) injury: The PTFL is the least commonly injured ligament in lateral ligament injuries of the ankle. It connects the talus bone to the fibula at the back of the ankle. PTFL injuries usually occur in severe ankle sprains or high-energy trauma.
CAUSES
Ankle sprain: The most common cause of a lateral ligament injury is an ankle sprain, which typically occurs when the foot rolls inward, resulting in stretching or tearing of the ligaments on the outer side of the ankle.
Sports injuries: Activities that involve quick changes in direction, jumping, or running on uneven surfaces increase the risk of ankle sprains and ligament injuries.
Trauma: Direct trauma or impact to the ankle joint, such as a fall or a collision, can cause damage to the lateral ligaments.
CLINICAL FEATURES
- Pain on the outer side of the ankle
- Swelling and bruising
- Difficulty walking or bearing weight on the affected foot
- Instability or a feeling of the ankle giving way
- Limited range of motion in the ankle joint.
RISK FACTORS
Body mass index, slow eccentric inversion strength, quick concentric plantar flexion strength, passive inversion joint position sense, and peroneus brevis reaction time were all linked to an elevated risk of lateral ankle injury.
ASSESSMENT OF ANKLE JOINT
- Amount of instability present by assessing the grade of the sprain;
- Loss of Range of motion (ROM);
- Loss of the muscle strength;
- Level of reduced Proprioception.
OBSERVATION
Any symptoms of injury, inflammation, skin colour changes, or muscle atrophy or hypertrophy are noted. Following that, the foot and ankle are observed in two separate positions: non-weight bearing and weight bearing. Take note of the gait pattern, degree of limp (if any), and facial expression when bearing weight.
HISTORY
Mechanism of injury: A plantarflexion/inversion injury would indicate damage to the lateral ligament, whereas a dorsiflexion/eversion injury would indicate damage to the medial ligament. Previous history of injury on the same side will give clues as to whether the ankle was unstable to begin with, or that a previous injury wasn’t properly rehabilitated.
History of injury on the other side as well may indicate a biomechanical predisposition towards ankle injuries.
GRADES
Grade 1: Mild sprain with minimal stretching or tearing of the ligament fibers. There may be slight swelling, tenderness, and minimal loss of function.
Grade 2: Moderate sprain with partial tearing of the ligament fibers. This grade is characterized by increased swelling, bruising, pain, and difficulty walking or bearing weight on the affected ankle.
Grade 3: Severe sprain with complete tearing or rupture of the ligament. Significant swelling, bruising, pain, and instability are commonly observed. Walking or weight-bearing may be extremely difficult or impossible.
SPECIAL TEST
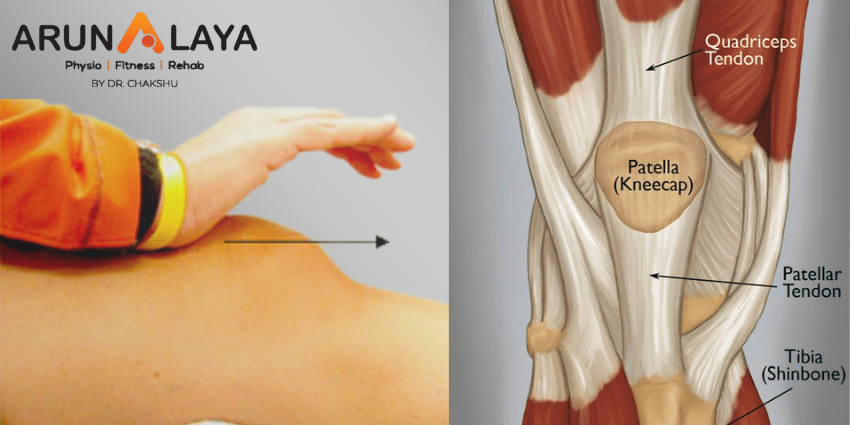
An anterior draw is performed to assess the ATFL and CFL integrity. The heel is grabbed with the ankle in plantarflexion, and the tibia is stabilised and dragged anteriorly.
The talar tilt is used to evaluate the integrity of the ATFL and CFL laterally, as well as the deltoid ligament medially. The heel is grabbed again, the tibia is stabilised, and the talus and calcaneus are pushed laterally and medially.
Beginning with a simple single leg stance, proprioception can be measured in a variety of more challenging methods. The patient can do it on the normal side first to give the therapist a sense of what is typical, and then try it on the injured side.
DIFFERENTIAL DIAGNOSIS
- Ankle fracture (medial/lateral malleolus, distal tibia/fibular)
- Damage to the medial ligament
- Dislocated ankle
- Other soft tissue damage (peroneal tendons, muscle strain)
TREATMENT
REDUCE PAIN AND SWELLING
The RICE regimen (Rest, Ice, Compression, and Elevation) can be used to minimise pain and swelling in the first 48-72 hours after an acute lateral ligament damage.
If weight bearing is too painful, the patient can use elbow crutches for 24 hours and remain non-weight bearing. However, it is critical to begin at least partial weight bearing as soon as possible, along with a regular heel-toe gait pattern, since this will help to reduce pain and swelling.
Gentle soft tissue massage and light stretches can be conducted to help with the clearance of oedema, as long as they are painless.
Range of motion exercises: These exercises aim to restore the normal range of motion in the ankle joint and may involve gentle ankle rotations, ankle pumps, and alphabet exercises.
Strengthening exercises: Strengthening the muscles around the ankle joint helps provide support and stability. Common exercises include calf raises, toe raises, ankle inversions and eversions (using resistance bands or manual resistance), and single-leg balance exercises.
Proprioceptive and balance exercises: These exercises improve the body’s awareness of joint position and enhance balance and stability. Examples include standing on one leg, balance board exercises, and wobble board exercises.
RETURN TO FUNCTIONAL ACTIVITY
- Twisting
- Jumping
- Hopping on one leg
- Running
- Figure of 8 running
Before returning to full functional activity the patient should have full range of pain free movement in the ankle, normal strength and normal proprioception. If returning to sports, the athlete should be encouraged to wear an ankle brace or to tape the ankle for a further 6 months to provide external support.