Deformities
Introduction
Deformities encompass a wide range of physical differences that can affect individuals from birth or develop over time due to injury, illness, or other factors. While deformities may vary in their appearance and impact, they are an intrinsic part of the diversity of the human experience. In this blog post, we’ll explore the complexities of deformities, dispel myths and misconceptions, and advocate for a more inclusive and accepting society.
Deciphering Deformities
Deformities can manifest in various forms and affect different parts of the body, including:
- Skeletal deformities: These involve abnormalities in the bones or joints, such as scoliosis (curvature of the spine), clubfoot (abnormal positioning of the foot), or limb length discrepancies.
- Craniofacial deformities: These affect the structure and appearance of the head and face, such as cleft lip and palate, craniosynostosis (premature fusion of skull bones), or micrognathia (undersized lower jaw).
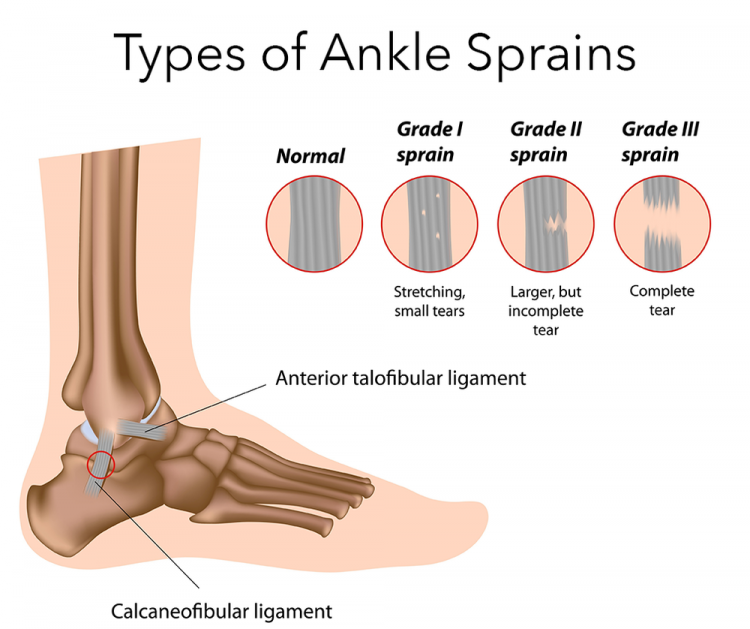
- Soft tissue deformities: These involve abnormalities in the muscles, tendons, ligaments, or skin, such as contractures (tightening of muscles and tendons), scars, or tissue overgrowth.
- Congenital deformities: These are present at birth and may result from genetic factors, prenatal exposures, or developmental anomalies, such as congenital heart defects, neural tube defects, or limb abnormalities.
Understanding the Impact of Deformities: Deformities can have a profound impact on individuals’ physical, emotional, and social well-being, affecting their self-esteem, body image, and quality of life. Some challenges associated with deformities may include:
- Physical limitations: Deformities may cause pain, discomfort, or difficulty performing daily activities, such as walking, dressing, or eating.
- Psychological effects: Individuals with deformities may experience stigma, discrimination, or negative perceptions from others, leading to feelings of isolation, shame, or depression.
- Social barriers: Deformities may impact social interactions, relationships, and opportunities for employment, education, or participation in community activities.
Promoting Inclusivity and Acceptance: Promoting inclusivity and acceptance of individuals with deformities requires a collective effort to challenge stereotypes, dismantle barriers, and foster a culture of empathy, respect, and dignity. Here are some ways to promote inclusivity and acceptance:
- Education and awareness: Increase awareness and understanding of deformities by providing accurate information, sharing personal stories, and challenging myths and misconceptions.
- Accessibility and accommodation: Ensure that environments, products, and services are accessible and accommodating for individuals with deformities, including physical accessibility, assistive devices, and adaptive technologies.
- Representation and visibility: Promote positive representation and visibility of individuals with deformities in media, advertising, and public spaces to celebrate diversity and challenge stereotypes.
- Advocacy and empowerment: Advocate for policies, programs, and initiatives that support the rights, inclusion, and well-being of individuals with deformities, including anti-discrimination laws, disability rights, and accessible healthcare services.
Support and community
Provide support networks, peer mentoring, and resources for individuals with deformities and their families to connect, share experiences, and access support services.
“At Arunalaya Healthcare, we pride ourselves on being the best physiotherapy center in Delhi. Our dedicated team of experts offers top-notch physiotherapy treatment tailored to your needs. Experience the difference with the leading physiotherapy clinic in Delhi area. Our commitment to excellence ensures that you receive the best physiotherapy care possible. Trust Arunalaya Healthcare for the best physiotherapy treatment in Delhi. Our advanced physiotherapy solutions set us apart as the premier choice for your rehabilitation needs. When it comes to physiotherapy, our center stands out as the best in Delhi. Choose Arunalaya Healthcare for comprehensive physiotherapy solutions that deliver results. Visit Arunalaya Healthcare today and discover why we are the best physiotherapy center in Delhi.