Multiple Sclerosis
Table Of Contents
- Introduction
- Unraveling the Complexity of Multiple Sclerosis
- Exploring the Spectrum of Symptoms
- Navigating Treatment Options and Coping Strategies
- Psychosocial support
Introduction
Multiple Sclerosis (MS) is a complex autoimmune condition that affects the central nervous system, causing a range of symptoms that can vary widely from person to person. As a chronic and often unpredictable disease, MS poses challenges for individuals and their families, requiring comprehensive management and support. In this blog post, we’ll delve into the intricacies of Multiple Sclerosis, explore its symptoms, treatment options, and coping strategies, and provide valuable insights for those impacted by this condition.
Unraveling the Complexity of Multiple Sclerosis
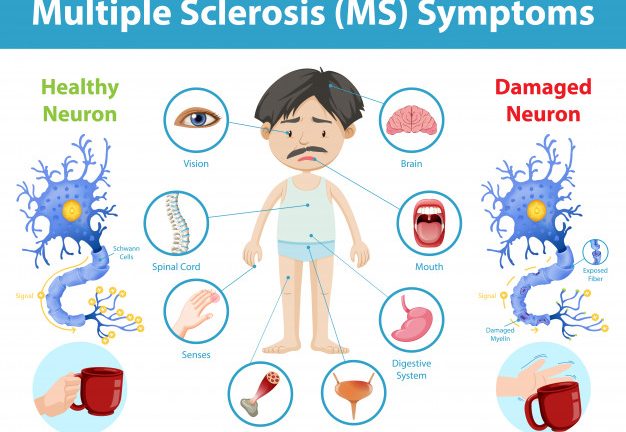
Multiple Sclerosis is characterized by the immune system mistakenly attacking the protective myelin sheath surrounding nerve fibers in the brain and spinal cord. This process, known as demyelination, disrupts the transmission of nerve signals, leading to a wide range of symptoms that can affect mobility, sensation, vision, cognition, and other bodily functions. While the exact cause of MS remains unknown, factors such as genetics, environmental triggers, and immune system dysfunction are believed to play a role in its development.
Exploring the Spectrum of Symptoms
The symptoms of Multiple Sclerosis can vary greatly depending on the location and severity of nerve damage within the central nervous system. Common symptoms may include:
- Fatigue: Debilitating fatigue is one of the most common and pervasive symptoms of MS, often described as overwhelming exhaustion that is not relieved by rest.
- Motor impairments: MS can cause muscle weakness, stiffness, tremors, coordination difficulties, and difficulties with balance and walking, affecting mobility and physical functioning.
- Sensory disturbances: Individuals with MS may experience numbness, tingling, or pain in various parts of the body, as well as changes in sensation, such as heightened sensitivity or loss of sensation.
- Visual disturbances: Optic neuritis, inflammation of the optic nerve, is a common manifestation of MS, leading to blurred vision, eye pain, double vision, or temporary vision loss.
- Cognitive changes: MS can impact cognitive function, causing difficulties with memory, concentration, problem-solving, and information processing, affecting work, relationships, and daily activities.
- Emotional changes: Mood swings, depression, anxiety, and other emotional changes are common in individuals with MS, often stemming from the challenges of living with a chronic and unpredictable condition.
Navigating Treatment Options and Coping Strategies
While there is no cure for Multiple Sclerosis, various treatment options are available to manage symptoms, slow disease progression, and improve quality of life. These options may include:
- Disease-modifying therapies: Medications, such as interferons, glatiramer acetate, or monoclonal antibodies, are prescribed to modify the immune response, reduce inflammation, and decrease the frequency and severity of relapses in relapsing-remitting MS.
- Symptom management: Symptomatic treatments may include medications, physical therapy, occupational therapy, speech therapy, or other interventions aimed at alleviating specific symptoms, such as fatigue, spasticity, pain, or bladder dysfunction.
- Lifestyle modifications: Adopting a healthy lifestyle that includes regular exercise, balanced nutrition, stress management, adequate sleep, and avoiding smoking and excessive alcohol consumption can help individuals with MS manage symptoms, improve overall well-being, and enhance quality of life.
- Supportive therapies: Complementary and alternative therapies, such as acupuncture, yoga, mindfulness meditation, or relaxation techniques, may offer additional benefits in managing symptoms, reducing stress, and promoting overall wellness.
Psychosocial support
Seeking support from mental health professionals, counselors, support groups, or online communities can help individuals with MS cope with emotional challenges, navigate lifestyle adjustments, and connect with others who understand their experiences.
“At Arunalaya Healthcare, we pride ourselves on being the best physiotherapy center in Delhi. Our dedicated team of experts offers top-notch physiotherapy treatment tailored to your needs. Experience the difference with the leading physiotherapy clinic in Delhi area. Our commitment to excellence ensures that you receive the best physiotherapy care possible. Trust Arunalaya Healthcare for the best physiotherapy treatment in Delhi. Our advanced physiotherapy solutions set us apart as the premier choice for your rehabilitation needs. When it comes to physiotherapy, our center stands out as the best in Delhi. Choose Arunalaya Healthcare for comprehensive physiotherapy solutions that deliver results. Visit Arunalaya Healthcare today and discover why we are the best physiotherapy center in Delhi.”
Lifestyle tips for living with MS | Multiple Sclerosis causes and symptoms | MS treatment options | Managing fatigue in MS | Coping with Multiple Sclerosis | Disease-modifying therapies for MS | Symptom management in Multiple Sclerosis | Emotional support for MS patients | Coping strategies for MS | Living with Multiple Sclerosis