Healing Hands: The Transformative Power of Manual Therapy in Physiotherapy
Introduction: Physiotherapy, also known as physical therapy, is a noble healthcare profession dedicated to optimizing physical function, preventing injuries, and aiding in the recovery process. At its core, physiotherapy employs a holistic approach to healing, and one of its most remarkable techniques is manual therapy. In this article, we will delve into the profound significance of manual therapy in the realm of physiotherapy, exploring its diverse techniques and the pivotal role it plays in patient treatment and rehabilitation.
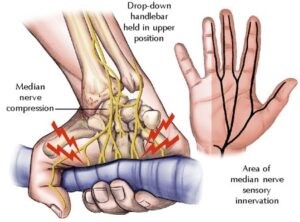
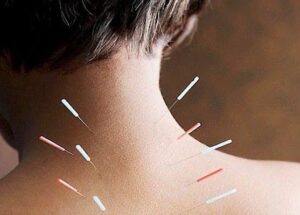
Understanding Manual Therapy: Manual therapy is an empathetic, hands-on approach to diagnosing, treating, and managing a myriad of musculoskeletal conditions and injuries. Skilled therapists employ their hands as instruments of healing, using precise movements and techniques to alleviate pain, enhance range of motion, and improve overall physical function. It stands as an indispensable component of physiotherapy, encompassing a range of techniques, each tailored to address unique patient needs.
Common Manual Therapy Techniques:
- Joint Mobilization: Therapists utilize controlled, gentle movements to promote optimal joint function. This technique is a lifeline for conditions such as osteoarthritis, effectively reducing joint stiffness and enhancing mobility.
- Joint Manipulation: Often referred to as “adjustments,” joint manipulation entails applying a controlled force to a joint, providing pain relief, restoring joint function, and realigning structures for improved overall well-being.
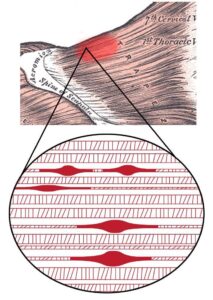
- Myofascial Release: Myofascial tissues envelop muscles, and therapists use this technique to release tension and restrictions within these tissues. Conditions like fibromyalgia and chronic pain find relief through myofascial release.
- Trigger Point Release: Therapists target specific trigger points within muscles, expertly applying pressure to alleviate pain and muscle knots. Conditions like tension headaches and myofascial pain syndrome greatly benefit from this technique.
The Role of Manual Therapy in Physiotherapy:
- Pain Relief: Manual therapy stands as a beacon of hope for individuals suffering from musculoskeletal pain, including back pain, neck pain, and joint discomfort. By addressing the root causes of pain, therapists empower patients to find relief without the need for medication or invasive procedures.
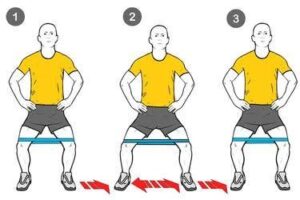
- Improved Range of Motion: For many patients grappling with injuries or chronic conditions, limited range of motion is a harsh reality. Manual therapy techniques such as joint mobilization and soft tissue massage act as catalysts for enhancing joint mobility and flexibility, offering the promise of functional movement.
- Injury Prevention: Manual therapy is not confined to treating existing injuries; it’s a staunch guardian against future ones. By identifying and rectifying biomechanical imbalances or weaknesses, therapists create tailored exercise and stretching regimens, substantially reducing the risk of injuries.
- Enhanced Functionality: Whether it’s aiding an athlete in recovering from a sports injury or assisting an elderly patient in regaining independence, manual therapy is instrumental in reinstating and elevating physical functionality.
- Patient-Centered Approach: Manual therapy places the patient at its heart. Physiotherapists evaluate each case individually, fashioning personalized treatment plans that ensure patients receive the most effective care tailored to their unique needs and conditions.
Conclusion: In the world of physiotherapy, manual therapy stands as a potent force for holistic healing and rehabilitation. Through techniques such as soft tissue massage, joint mobilization, and myofascial release, compassionate therapists hold the power to alleviate pain, enhance mobility, and improve overall physical function. By amalgamating manual therapy with exercise, education, and lifestyle modifications, physiotherapists empower patients to take charge of their recovery, ultimately achieving enduring results. The healing hands of manual therapy serve as an invaluable resource on the path to enhanced health and well-being.